Difference Between Yeast Infection and Bacterial Vaginosis BV
Both yeast infections and bacterial vaginosis are vaginal infections and are common causes of vaginal discharge, but the two infections and medical conditions are not the same, and they require different treatments.
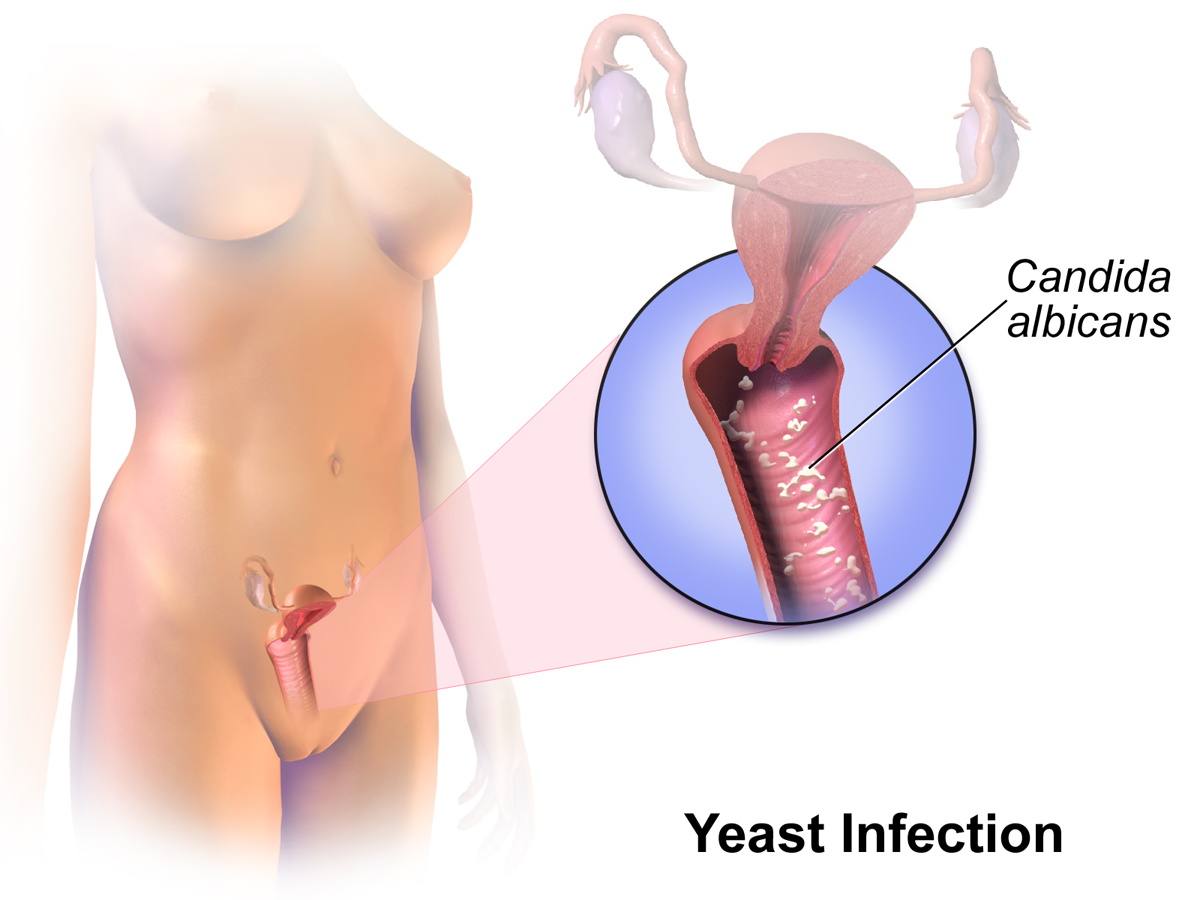
What is Yeast infection?
75% of women get at least one yeast infection during their life time. This is caused by overgrowth of natural yeast in the vagina and is known as Candidal vaginitis. The infection causes heavy cottage cheese like discharge and causes itching.
A vaginal yeast infection is a fungal infection that results in itching, heavy discharge, swelling around vagina and irritation. Vaginal yeast infection is also called vaginal candidiasis and affects up to three out of four women. Many women suffer twice or even more. Although a vaginal yeast infection is not transmitted sexually, yet one can spread the fungus through mouth or the genital contact. There are several treatments and medications that can cure vaginal yeast infections.
What is Bacterial Vaginosis?
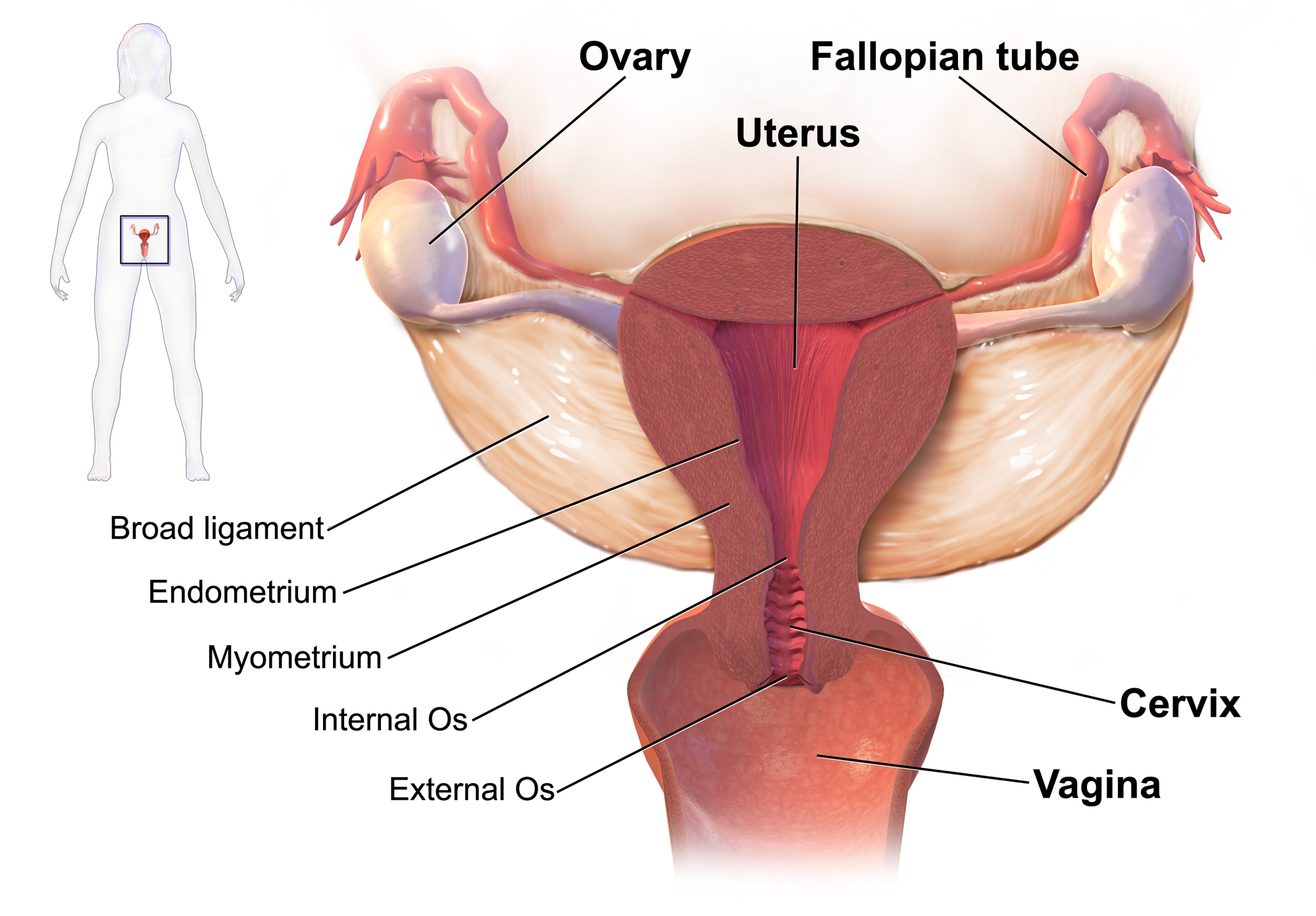
It is a mild infection of the vagina. It is normally a mild problem that vanishes by itself after few days. However, it could lead to some serious health conditions, if not treated. Vagina has lactobacilli bacteria that has the tendency to keep other harmful bacteria at a distance. However, when the vagina is invaded by anaerobic bacteria, they kill off lactobacilli bacteria resulting in heavy vaginal discharge, burning and itching. The discharge could have a fishy odour, especially after being exposed to anything that could potentially increase body pH, such as semen or menstrual fluid. It is diagnosed by doing a pelvic exam and by taking a sample of the vaginal discharge. It is more common in women who are sexually very active as it is often transmitted through sexual intercourse. The risk of getting this infection is higher if you have more than one sexual partners and if you douche. If you have this infection when you are pregnant, it can cause miscarriage, preterm delivery and even uterine infection.
Difference between Yeast infection and Bacterial Vaginosis
Etiology
Yeast infection
The infection is caused by Candida species known as candida albicans.
Bacterial Vaginosis
Infection is caused by Gardnerella vaginalis, Mobiluncus species, Trichomonas vaginalis, Mycoplasma hominis and Urea plasma.
Pathophysiology
Yeast infection
The infection takes place inside the mouth, intestines, vagina and on the skin.
Bacterial Vaginosis
It is a synergistic infection involving not only Gardnerella vaginalis but several anaerobic bacteria as well.
Common symptoms
Yeast infection
Itching, Soreness, redness, rash, pain during intercourse. Whitish gray, watery and clumpy vaginal discharge is also a tell-tale symptom.
Bacterial Vaginosis
Heavy discharge (cloudy, bloody, yellow or green) vaginal pain and burning, abnormal consistency of vaginal fluid. The vaginal discharge and odour are often more noticeable after sexual intercourse.
Treatment
Yeast infection
Prescription antifungal agents. Common medications include; Butoconazole, Flucanozole (Diflucan), Itraconazole, Miconazole (Lotrimin), Monistat, Terconazole (Terazol). Possible treatments for extreme or complicated yeast infections include, 14-day cream or ointment or even suppository vaginal treatment.
Bacterial Vaginosis
Prescription antibiotic agents. Common medications include; Clindamycin, Tinidazole, Metronidazole
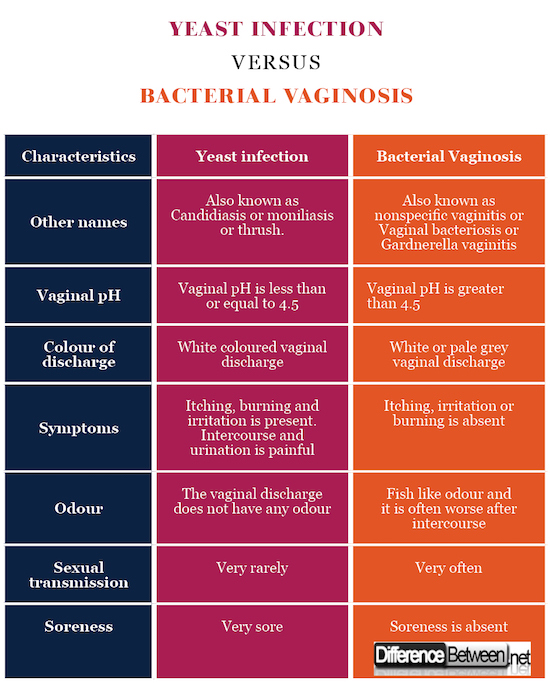
Vaginal discharge
Yeast infection
Vaginal discharge is curdy white, Cottage cheese like and sometimes increased.
Bacterial Vaginosis
Vaginal discharge may be increased in case of bacterial infection. It is white, thin, homogenous and grey coloured adherent.
Vaginal pH
Yeast infection
Vaginal pH is > 4.5 usually.
Bacterial Vaginosis
Vaginal pH is > 4.5.
KOH prep
Yeast infection
Pseudohyphae seen
Bacterial Vaginosis
Positive Whiff test
Amine odour
Yeast infection
Odour is virtually non-existent.
Bacterial Vaginosis
Fishy unpleasant odour is present
Soreness
Yeast infection
Very sore
Bacterial Vaginosis
Soreness is absent
Consistence
Yeast infection
Cottage cheese like.
Bacterial Vaginosis
Milky or creamy and thin viscosity.
Wet mount test
Yeast infection
Yeast buds or spores or hyphae can be seen. Wet mount examination reveals budding yeast and/or Pseudo hyphae. Here also WBC’s are seen.
Bacterial Vaginosis
On wet preparation of vaginal discharge, White blood cells are present and stippled epithelial cells support a diagnosis of bacterial vaginosis.
Risk factors
Yeast infection
Physiological – Pregnancy, infancy
Hematological – AIDS, Cellular immune deficiency, Leukemia, Aplastic Anemia, Lymphoma.
Iatrogenic – Antibiotics, Oral Contraceptives, Chemotherapy.
Uncontrolled diabetes or using oral birth control or estrogen hormone therapy. Douching, antibiotics, vaginal sprays, or steroid therapies and a weak immunity system also maximises the risk of contracting a yeast infection.
Bacterial Vaginosis
Increased number of sexual partners, Cigarette smoking, douching, Lack of condom use, Intrauterine device etc.
Examinations
Yeast infection
Physical examination
- Thick and white discharge adhering to walls of vagina.
- Vulvar and vaginal erythema
- Fissures
- Edema
Bacterial Vaginosis
Physical examination
- Appearance of tissue
- Discharge with no colour
- Abnormal odour
- Homogenous discharge adhered to walls of vagina
Summary of Difference between Yeast Infection and Bacterial Vaginosis
The points of difference between Yeast Infection and Bacterial Vaginosis have been summarized below in tabular form:
Yeast infection Vs. Bacterial Vaginosis
- Difference Between Vaccination and Immunization - March 3, 2024
- Difference Between Selective Mutism and Autism - February 25, 2024
- Difference Between Depersonalization-Derealization and Dissociation - January 18, 2024
Search DifferenceBetween.net :
Leave a Response
References :
[0]Badiee, P., & Hashemizadeh, Z. (2014). Opportunistic invasive fungal infections: diagnosis & clinical management. The Indian journal of medical research, 139(2), 195.
[1]Badiee, P., & Hashemizadeh, Z. (2014). Opportunistic invasive fungal infections: diagnosis & clinical management. The Indian journal of medical research, 139(2), 195. Bilardi, J. E., Walker, S., Temple-Smith, M., McNair, R., Mooney-Somers, J., Bellhouse, C., ... & Bradshaw, C. (2013). The burden of bacterial vaginosis: women’s experience of the physical, emotional, sexual and social impact of living with recurrent bacterial vaginosis. PloS one, 8(9), e74378.
[2]Mulu, W., Yimer, M., Zenebe, Y., & Abera, B. (2015). Common causes of vaginal infections and antibiotic susceptibility of aerobic bacterial isolates in women of reproductive age attending at Felegehiwot referral Hospital, Ethiopia: a cross sectional study. BMC women's health, 15(1), 42.
[3]Image credit: https://upload.wikimedia.org/wikipedia/commons/8/84/Yeast_Infection.png
[4]Image credit:
[5]Image credit: https://en.wikipedia.org/wiki/Pelvic_inflammatory_disease#/media/File:Blausen_0732_PID-Sites.png