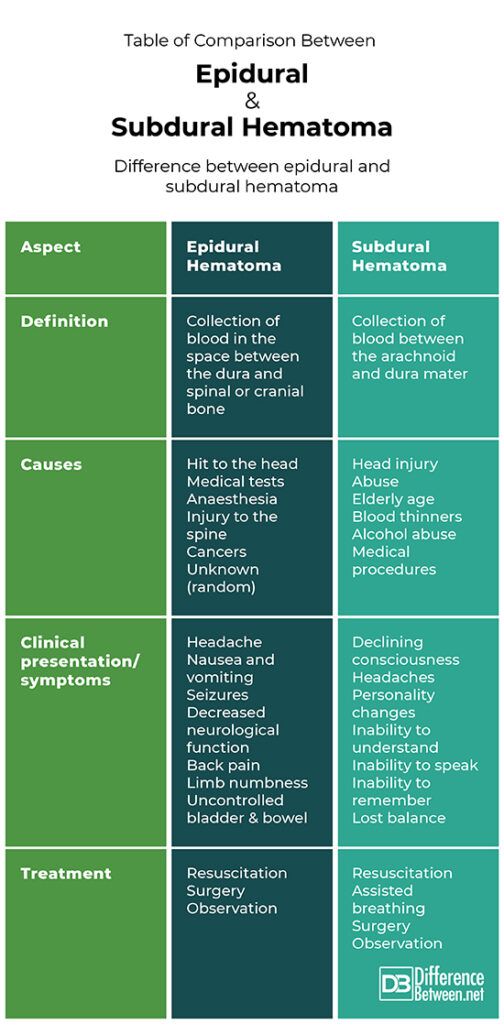
Difference Between Epidural and Subdural Hematoma
Introduction
The human brain is covered by a few layers of membranes for protection. These three layers are called the meninges. The delicate inner layer is the pia mater, the middle layer is the arachnoid (filled with fluid to cushion the brain) and the final outer layer is called the dura mater.
A hematoma refers to the abnormal occurrence of blood outside of its usual blood vessel. Subdural and epidural hematomas are therefore both types of collections of blood within two different spaces relating to the brain or spinal cord.

This article will look into the brainy matter and help differentiate the two from each other!
Definition and Pathophysiology
An epidural hematoma is the collection of blood in the space between the dura and spinal or cranial bone. Intracranial epidural hematoma (the one between the dura and the cranial bones) is the most serious complication of a head injury and needs to be urgently diagnosed and treated. This type of hematoma may also be acute (it happened quickly), subacute (it happened relatively recently) or chronic (it has been happening over a longer period of time).
A subdural hematoma refers to the collection of blood between the arachnoid and dura mater. A subdural hematoma is an outcome most common in traumatic head injuries.
Causes
Epidural hematomas are generally seen after a type of hit to the head. This hit causes the periosteal dura to separate itself from bone. Spinal epidural hematomas can happen out of the blue or after a minor trauma, such as a lumbar puncture test or after receiving an epidural anaesthesia. In some cases, cancers can cause epidural hematomas, as well as injury to the spine (like a herniated disk).
Subdural hematomas are most often seen in patients that have experienced a severe head injury but can also occur in the elderly, and on occasion in patients on blood thinners. This hematoma can also occur out of the blue or be caused as a complication of a medical procedure. It has been noted that severe alcoholism can contribute to blood thinning and be a cause of subdural hematomas.
Sadly, child abuse such as shaken baby syndrome can also cause a subdural hematoma.
Clinical Presentation and Symptoms
Epidural hematomas should, out of safety, be suspected or expected in a person who has sustained a form of head trauma. Patients usually show a conscious time between the impact and the first time they lose consciousness. After that, there is a slow decline in mental status. General symptoms tend to include the presence of a headache, nausea and vomiting, the patient may experience seizures and present with obvious neurological deficits. Spinal epidural hematomas usually present with severe back pain in a specific area and sometimes include weakness, numbness, or the inability to control bladder and stool movement.
The presentation of subdural hematomas depends on where it has occurred and how fast it is developing. Some patients with this injury stay conscious but other patients deteriorate over time as the bleeding gets worse. The clinical symptoms in subdural hematomas generally include a declining consciousness, presence of a severe headache, loss of balance functions, personality changes or the inability to speak and remember anything.
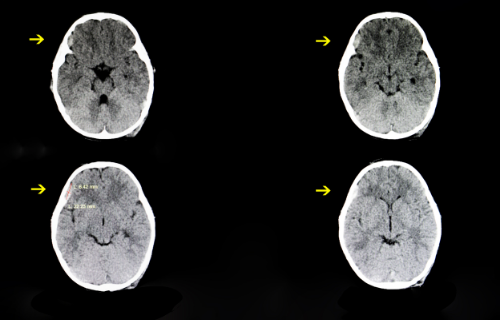
Diagnosis
Epidural hematomas can be diagnosed through medical tests. These tests include scans such as non-contrast CT scanning of the head to see skull fractures and the epidural hematoma itself. MRI scans also clearly show an epidural hematoma, though it may not be the go-to test for unstable patients. Toxicology and alcohol blood tests can be done to rule out other causes.
An emergency CT scan of the head must be performed when an acute subdural hematoma is suspected (once the patient is stabilised, of course). A non-contrast CT of the head is also effective in making a diagnosis. Drug and alcohol screenings are also optional tests to rule out other causes.
Treatment
The treatment of an epidural hematoma is done depending on the cause and the severity. In severe cases resuscitation might be necessary, including surgery to remove the bleed (a craniotomy or laminectomy).
Patients with a small bleed can be treated with observation and bleeding may absorb over time and resolve.
Subdural hematomas are treated on the level of severity and per the cause. In severe cases resuscitation is needed. Emergency surgery (decompression surgery) can be performed and patients with a certain coma score are often assisted with breathing.
Patients with a small bleed and a minor headache can be treated under observation.
Table of comparison between epidural and subdural hematoma
Summary
Both subdural and epidural hematomas are collections of blood in different locations within the skull or spinal cord. Acute subdural hematomas have the lowest rate of survival in comparison to epidural hematomas. It is critically important that medical care should be urgently given after a traumatic head injury or a suspected bleed in the brain or spinal cord. This is because of severe consequences that can occur when there is a hematoma that is not treated in time!
FAQ
What is the difference between subdural hematoma and subdural hemorrhage?
A hematoma refers to the collection of already clotted or semi-clotted blood, where hemorrhage refers to active bleeding contributing to a hematoma.
Can an epidural cause a subdural hematoma?
Most people also have a skull fracture after a traumatic head injury. Because of this, epidural hematomas may occur in combination with subdural hematomas. If this is not the case, then they generally occur alone.
What is epidural and subdural hemorrhage?
An epidural hemorrhage is the active bleeding in the space between the dura and spinal or cranial bone. A subdural hemorrhage refers to the active bleeding between the arachnoid and dura mater.
Is epidural or subdural hematoma more common?
Intracranial epidural hematomas occur in around 2% of patients with severe head injuries, whereas acute subdural hematomas tend to occur in 5-25% of patients with severe head injuries. Therefore, acute subdural hematomas are more commonly seen.
- Difference Between a Cochlear Implant and Normal Hearing - October 4, 2022
- Difference Between Obstructive and Restrictive Spirometry - September 11, 2022
- The Difference Between White Box and Black Box Testing - September 11, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Bir, S.C., Maiti, T.K., Ambekar, S and Nanda, A. “Incidence, hospital costs and in-hospital mortality rates of epidural hematoma in the United States”. Clinical Neurology and Neurosurgery, vol. 138, 2015, pp. 99-103
[1]Cohen, M and Scheimberg, I. “Subdural haemorrhage and child maltreatment”. Lancet, vol. 373, no. 9670, 2009, pp. 1173-1174.
[2]Corbett, S., Bultitude, M., Gossage, J., Burnand, K and Lahiri, R. Browse's introduction to the symptoms and signs of surgical disease.
[3]Meagher, Richard and Lutsep, Helmi. Subdural Hematoma. https://emedicine.medscape.com/article/1137207-overview
