Difference Between Diabetic Ulcer and Pressure Ulcer
A diabetic ulcer is a sore that develops on the foot of a person with diabetes. A pressure ulcer is a sore that develops on a part of the body where there is a bony projection pressing against a firm surface.
What is Diabetic Ulcer?
Definition:
A diabetic ulcer is a sore that usually forms on the foot of a person who has diabetes, and which can become gangrenous leading to amputation of the limb.
Symptoms:
The main symptom is the presence of a sore that is painful when touched. The sore also often has a discharge that can be foul- smelling. The sore on the foot often ulcerates and becomes infected, which can cause the foot to swell and become red in color. The infection can also cause you to have a fever if it is very bad.
Complications:
A diabetic foot ulcer can become gangrenous and this infection can spread leading to amputation of the foot or even the leg. In extreme cases, a person can die from bacteremia (bacteria in the bloodstream) leading to septic shock and even death.
Diagnosis:
Diagnosis is by physical examination in which the integrity of the skin is checked and the entire foot, including your toes and toenails, are carefully examined for signs of injury or blistering of the skin. Doctors may also test the level of blood flow by measuring blood pressure in the arteries of the leg and foot using a Doppler probe. This can indicate if there are blood vessel problems that could be causing an ulcer to develop, or increase the likelihood of such a problem occurring.
Risk factors:
Having poorly controlled diabetes leading to diabetic neuropathy (damaged nerves) is the main risk factor for diabetic ulcers. High blood sugar levels damage the nerves and so you do not feel when you have a sore on your foot. Another risk factor is not being careful and checking your feet often, especially if you have bought new shoes which could give you a blister or callus which could become an ulcer. Peripheral artery disease in patients with diabetes is another risk factor resulting in compromised blood flow.
Treatment:
The ulcer often needs to be washed and any dead tissue removed in a process called debridement. Antibiotics may need to be given to stop any infection. Antibiotics such as clindamycin or penicillin or cephalexin may be used. Wearing special footwear can also help to prevent ulcers from becoming worse or to prevent further ulceration. Where blood vessels are blocked due to arterial disease, vascular surgery may be needed.
What is Pressure Ulcer?
Definition:
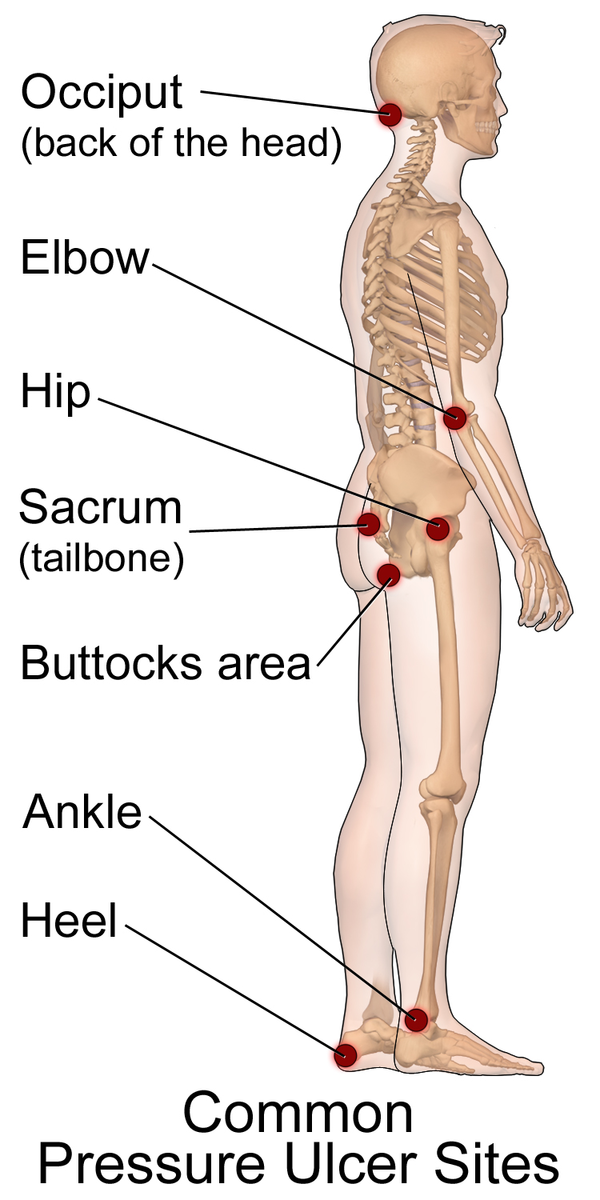
A pressure ulcer is also known as a decubitus ulcer and is a region of tissue that has become damaged and necrotic (dying). It most often happens where skin over bone is pressed against a hard surface for an extended time period.
Symptoms:
The area where the ulcer starts to develop first appears reddish and may feel warm or different from normal in some way. The skin then starts to blister and eventually the skin erodes away down into the subcutaneous layer and in extreme cases, down to the bone.
Complications:
Left untreated a pressure ulcer can result in osteomyelitis in which the bone becomes infected. Cellulitis is also a complication that can lead to bacteria in the bloodstream, which can even result in sepsis and death.
Diagnosis:
The diagnosis is based on a physical exam and the degree of the ulcer is staged according to how far it has developed, with stage 1 being the least severe and stage 4 being the most severe. Photos may be taken to track the progress of the wound.
Risk factors:
Risk factors for pressure ulcers include being older than 65, having a compromised circulatory system and being mainly immobile. Being bedridden for whatever reason is a very big risk factor for developing decubitus ulcers.
Treatment:
Treatment includes reducing pressure on the area by changing the position of the patient when they are bedridden or using some type of support such as pillows or other padding. Bedridden patients do need to be turned often because of the risk of pressure ulcers. The ulcers need to be cleaned with antiseptics and water, and any dead tissue needs to be removed. Wounds need to be bandaged and antibiotic ointments can be applied. In some cases, an antibiotic given internally may be needed. Ointments that contain polymyxin B, metronidazole or mupirocin can be used.
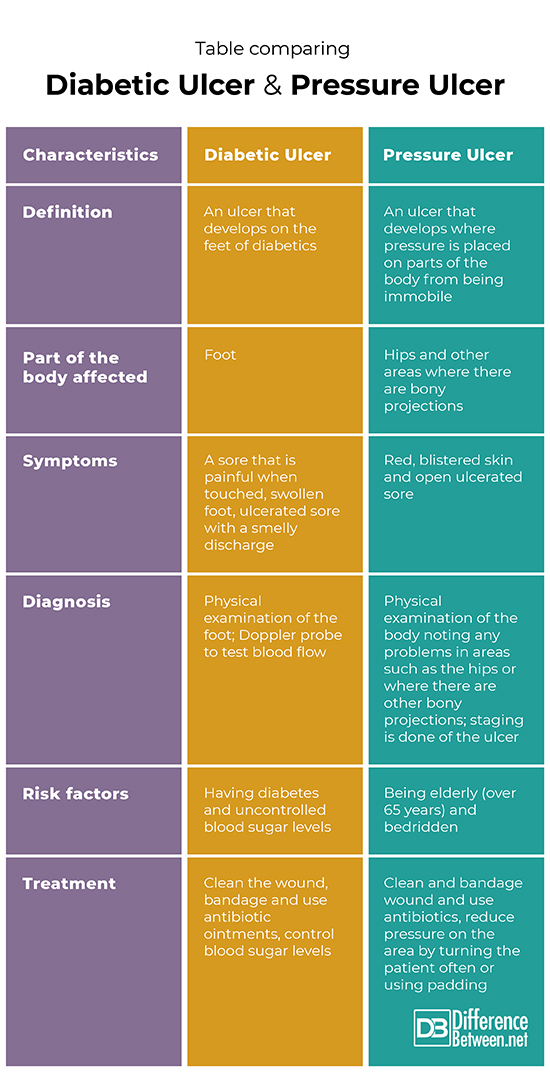
Difference between Diabetic ulcer and Pressure ulcer?
Definition
A diabetic ulcer is a sore that develops on the foot of a person with diabetes. A pressure ulcer is a sore that develops where bony projections are pushed against firm surfaces and occurs in bedridden or immobile patients.
Part of the body affected
A diabetic ulcer affects the feet. A pressure ulcer affects bony areas of the body like the hips.
Symptoms
The symptoms of a diabetic ulcer are a sore on the foot which often has a bad-smelling discharge and may be painful if touched, and the foot may swell. Symptoms of a pressure ulcer are a painful sore, blistered, red and swollen skin and ulceration.
Diagnosis
A diabetic ulcer is diagnosed by physical exam and Doppler flow of blood. A pressure ulcer is diagnosed by physical exam.
Risk factors
The risk factors for a diabetic ulcer include having diabetes with badly controlled blood sugar levels and having arterial disease. The risk factors for pressure ulcers are being elderly (over 65) and being largely immobile or bedridden.
Treatment
Diabetic ulcers are treated with antibiotics and removing dead tissue, and by controlling blood sugar levels and wearing the correct footwear. Pressure sores are treated by providing support and padding, moving the person often, using antibiotics and removing dead tissue.
Table Comparing Diabetic Ulcer and Pressure Ulcer
Summary of Diabetic Ulcer Vs. Pressure Ulcer
- Both diabetic and pressure ulcers are sores that if left untreated can lead to bacteremia, sepsis, and death.
- Diabetic ulcers occur on the feet of the patient.
- Pressure ulcers occur on the parts of the body where there are bony projections.
- In both types of ulcers, wounds need to be cleaned, dead tissue removed and often antibiotics given.
- Difference Between Rumination and Regurgitation - June 13, 2024
- Difference Between Pyelectasis and Hydronephrosis - June 4, 2024
- Difference Between Cellulitis and Erysipelas - June 1, 2024
Search DifferenceBetween.net :
Leave a Response
References :
[0]Alexiadou, Kleopatra, and John Doupis. "Management of diabetic foot ulcers." Diabetes Therapy 3.1 (2012): 4.
[1]Cavanagh, Peter R., et al. "Treatment for diabetic foot ulcers." The Lancet 366.9498 (2005): 1725-1735.
[2]Kroshinsky, Daniela, and Lauren Strazzula. “Pressure ulcers (Bedsores; Decubitus Ulcers; Decubiti; Pressure Sores)”. Merckmanuals. Merck & Co., 2017, https://www.msdmanuals.com/professional/dermatologic-disorders/pressure-ulcers/pressure-ulcers?query=diabetic%20ulcer
[3]Image credit: https://commons.wikimedia.org/wiki/File:Pressure_Ulcer_Sites.png
[4]Image credit: https://en.wikipedia.org/wiki/Impetigo#/media/File:Bullous_impetigo1.jpg