Difference Between Mullerian Anomalies Agenesis and Androgen Insensitivity
What is Mullerian Anomalies agenesis and androgen insensitivity?
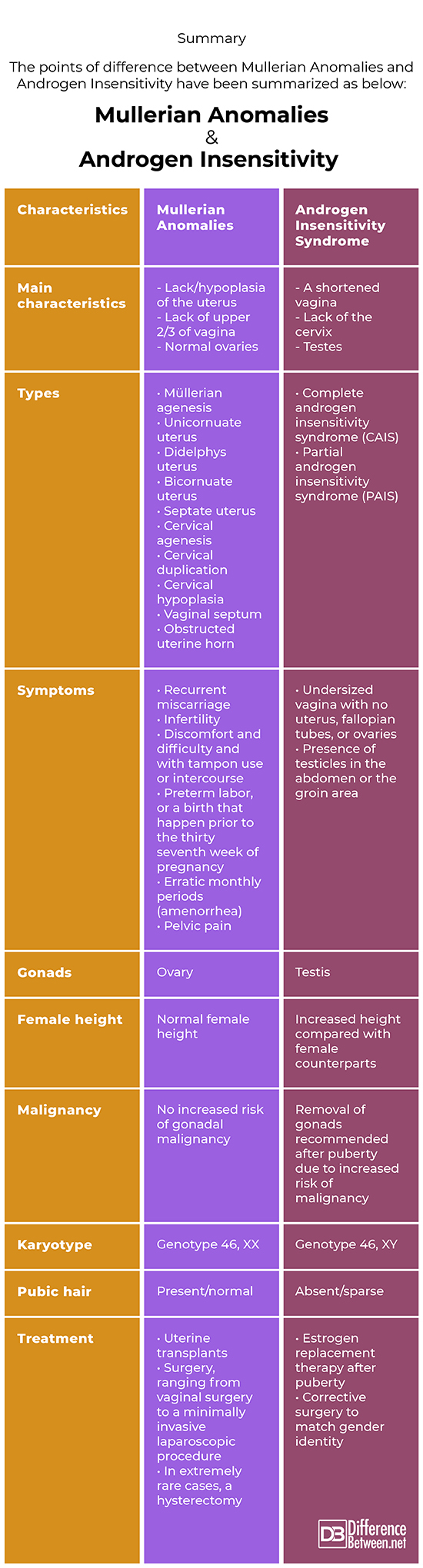
Müllerian agenesis is a rare medical condition that affects females. In this condition, the vagina and the uterus do not develop fully in females who have normal ovarian function and normal external genitalia. Androgen insensitivity is a genetic condition that involves hormonal resistance because of androgen receptor dysfunction.
Similarity
Both are developmental defects resulting in primary amenorrhea.
Mullerian Anomalies
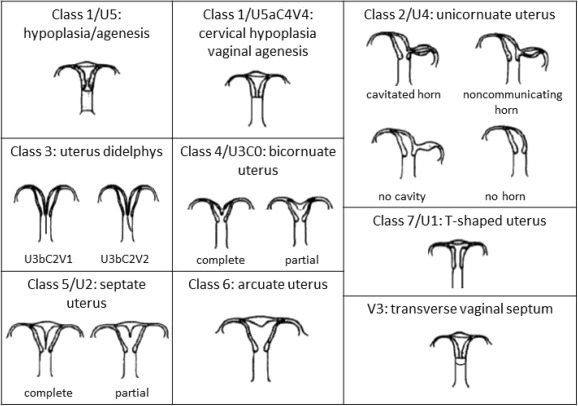
Müllerian agenesis (Mayer‐Rokitansky‐Küster‐Hauser syndrome) is caused by inadequate development of embryo of the müllerian duct, with resultant atresia of the vagina, uterus, or both. The passage or canal of the vagina is significantly shortened and appears as a small depression underneath the urethra.
Androgen Insensitivity
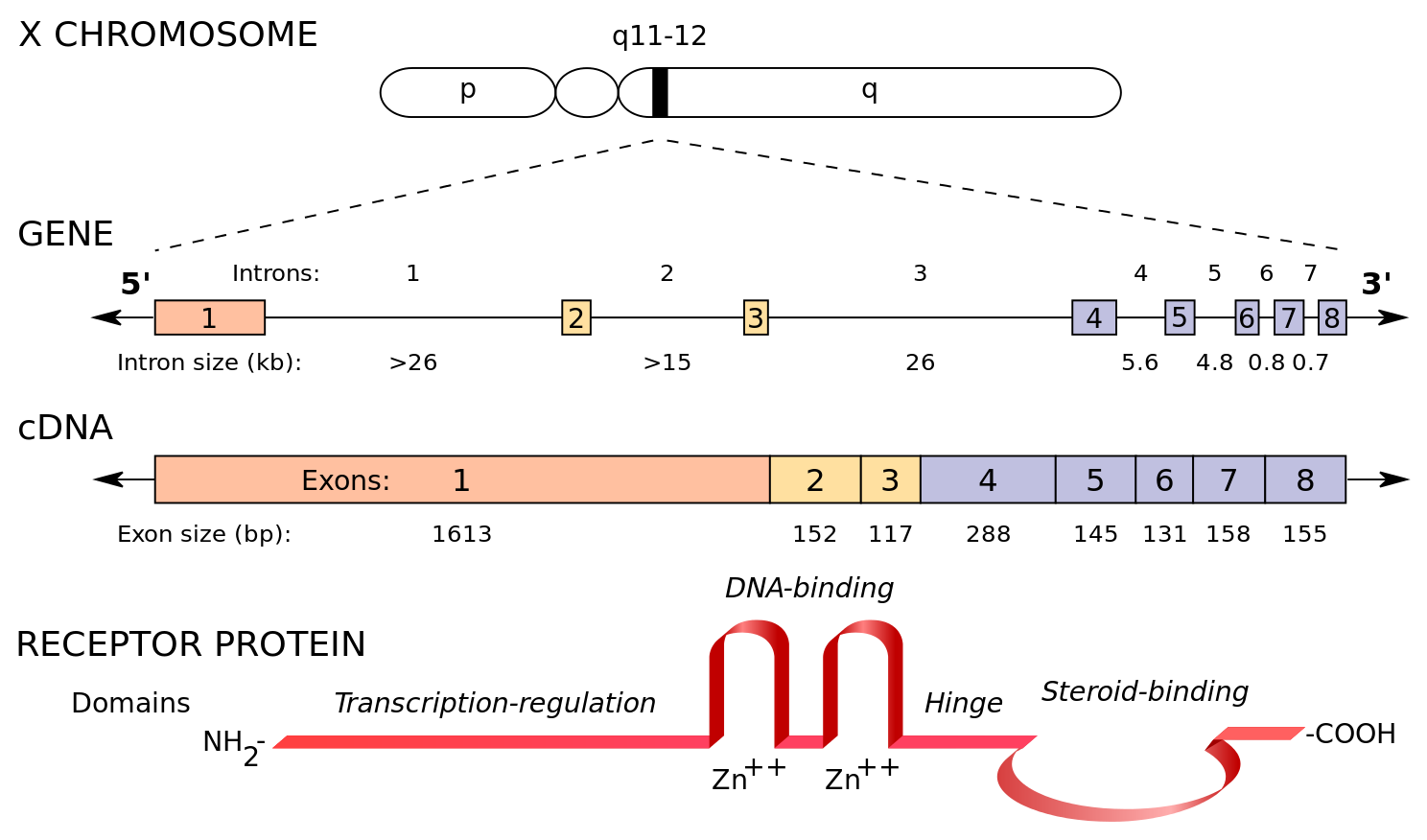
Androgen insensitivity syndrome (AIS) is when a human who is genetically a man (possessing one X and one Y chromosome) is averse to androgens (male hormones) person who is genetically male (who has one X and one Y chromosome) is resistant to male hormones (called androgens). As a result, the individual has some of the physical traits of a female, but the genetic features of a man.
Difference between Mullerian Anomalies and Androgen Insensitivity
Definition
Mullerian Anomalies
Müllerian anomalies affect up to 4% of women. The anomaly is basically a ‘congenital disorder’ which means that this problem occurs at the time of fetal development and is present at birth.
Müllerian anomalies occur when müllerian ducts develop abnormally, which can become a reason to cause disruption in the development of the full reproductive organs – fallopian tubes, cervix, uterus, and upper 2/3rd of the vagina
Androgen Insensitivity
Androgen insensitivity syndrome occurs when body is unable to use androgen hormones. Individuals with this condition are usually men, with one X chromosome and one Y chromosome in every single cell. This condition affects the sexual development prior to birth and at the time of puberty. Because people with this condition are not able to be responsive to specific male sex hormones termed as androgens. They possess female external sex features of both men and women sexual development.
Individuals with this condition have the external sex characteristics of women, but lack a uterus and hence do not have monthly cycle and are not able to become pregnant (infertile).
Causes
Mullerian Anomalies
Some causes may be hereditary and some may be attributed to a random gene mutation or developmental defect.
Androgen Insensitivity
It is caused by the genetic alteration or mutations on the X chromosome that means the body is not able to respond to testosterone either completely or partially.
Symptoms
Mullerian Anomalies
- Infertility
- No menstrual cycle
- Infertility
- Recurrent miscarriage.
- Preterm labour
- Pelvic pain
- Difficulty with intercourse
Androgen Insensitivity
- No periods
- Breasts development
- Growth spurts as normal
- Slightly taller than a usual girl
- No pubic hair or very little pubic hair
Diagnosis
Mullerian Anomalies
- Pelvic ultrasound
- Pelvic magnetic resonance imaging (MRI)
- Hysterosalpingography
- Hysteroscopy
- Vaginoscopy
- Laparoscopy
Androgen Insensitivity
- Genetic testing
- Pelvic ultrasound
- Blood test to assess the testosterone levels – luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
Summary
The points of difference between Mullerian Anomalies and Androgen Insensitivity have been summarized as below:
FAQ
Why ovaries are normal in Mullerian Anomalies agenesis?
Because ovaries don’t develop from the primordial anlage of the female reproductive tract (Müllerian ducts), impacted individuals may have normal secondary sexual traits but are infertile because of the absence of functional uterus. However, becoming a parent is possible by means of gestational surrogates.
Can you get pregnant with Mullerian Anomalies agenesis?
Yes. Assisted reproductive procedures with application of a gestational carrier (surrogate) have been reported to be victorious for women with müllerian agenesis. Female offspring or child of women who conceived by assisted reproductive technique usually have normal fallopian tubes, the uterus, the vagina, although familial aggregates of müllerian have been reported
How is vaginal agenesis diagnosed?
Vaginal agenesis, in some cases can be diagnosed by physical examination. Other tests include an ultrasound (to assess whether ovaries and uterus are present and location of your kidneys), an X-ray (to check skeletal anomalies), or MRI (to check reproductive tract and kidneys).
Blood tests may also be done to assess chromosomes and evaluate hormone levels
How is MRKH diagnosed?
MRKH or Mayer–Rokitansky–Küster–Hauser syndrome or vaginal agenesis are the same. The diagnosis involves physical examination. Other tests include an ultrasound (to assess whether ovaries and uterus are present and location of your kidneys), an X-ray (to check skeletal anomalies), or MRI (to check reproductive tract and kidneys).
Blood tests may also be done to assess chromosomes and evaluate hormone levels
What is Mullerian Anomalies syndrome?
Müllerian duct anomalies syndrome includes structural anomalies triggered by errors in müllerian-duct development at the time of spatial distribution of cells during the embryonic development of an organism called embryonic morphogenesis. Factors that precipitate include genetics, and maternal exposure to teratogens.
Do people with MRKH syndrome have periods?
No. People with MRKH syndrome typically do not get monthly menstrual cycles since their reproductive organs are either compromised or absent
- Difference Between Global Warming and Greenhouse Effect - May 18, 2024
- Difference Between Vaccination and Immunization - March 3, 2024
- Difference Between Selective Mutism and Autism - February 25, 2024
Search DifferenceBetween.net :
Leave a Response
References :
[0]Chandler, T., Machan, L. S., Cooperberg, P. L., Harris, A. C., & Chang, S. D. (2009). Müllerian duct anomalies: from diagnosis to intervention. The British journal of radiology, 82(984), 1034-1042.
[1]Folch, M., Pigem, I., & Konje, J. C. (2000). Müllerian agenesis: etiology, diagnosis, and management. Obstetrical & gynecological survey, 55(10), 644-649.
[2]Gottlieb, B., Pinsky, L., Beitel, L. K., & Trifiro, M. (1999). Androgen insensitivity. American journal of medical genetics, 89(4), 210-217.
[3]Hughes, I. A., Werner, R., Bunch, T., & Hiort, O. (2012, October). Androgen insensitivity syndrome. In Seminars in reproductive medicine (Vol. 30, No. 05, pp. 432-442). Thieme Medical Publishers.
[4]Image credit: https://ars.els-cdn.com/content/image/1-s2.0-S1028455920300036-gr1.jpg
[5]Image credit: https://commons.wikimedia.org/wiki/File:Functional_domains_of_the_human_androgen_receptor.svg
