Difference Between Spirometry and Peak Flow Meter

Spirometry is a simple test performed by medical practitioner. It is used to measure pulmonary or lung functioning or the amount of air inhaled and exhaled as well as the speed of exhalation (Mayo Clinic). The test is used to diagnose diseases that affect breathing like asthma, chronic bronchitis, chronic obstructive pulmonary disease, pulmonary fibrosis, and emphysema. It may also be used to check the efficacy of a prescribed medication, whether the lung function is adequate prior to surgery, or to screen for lung disorders related to a person’s occupation. A doctor may order spirometry if a patient is wheezing, suffers from shortness of breath, or has a chronic cough (American Lung Association).
A peak flow meter, on the other hand, is an inexpensive, easy-to-use, portable device that measures with what force a person expels air from their lungs. It is considered useful for asthmatics because it enables the sufferer to decide whether to take quick-relief medication and/or a trip to the emergency room, as well as identifies triggers for asthma attacks in terms of location and time of day (American Lung Association).

How Spirometers and Peak Flow Meters Work
A spirometer is a device that is found in a medical practitioner’s office, and spirometry, the test, takes about 15 minutes. It requires the patient to breath into a tube attached to the device. The patient exhales into the tube as hard as he or she can for several seconds at least three times. The highest value obtained is considered the result (Mayo Clinic). The key measurements include forced vital capacity (FVC), which is the largest amount of air forcefully exhaled, and forced expiratory volume (FEV1), which is the largest amount of air the patient can force from their lungs in one second. Normal values are calculated based on age, height, and gender (American Lung Organization), and the lower the readings, the more restricted the breathing and more significant the obstruction (Mayo Clinic). A normal test result is 80%. Doctors often also calculate the FEV1:FVC ratio, which represents the percentage of a patient’s lung capacity exhaled in 1 second. If a patient’s results are abnormal, other tests are performed, for example, chest and sinus X-rays and blood tests (Erica Cirno).
Like the spirometer, a peak flow meter is a device that tests three breathes, and the highest reading of three readings is considered the valid reading. Like a spirometer, a normal reading is considered 80 to 100 percent, while less than 50 percent is considered a medical alert (American Lung Association). The peak flow meter, however, is limited to measuring the highest force with which a person exhales rather than their lung capacity.
Risks, exclusions, and limitations
A spirometry requires some exertion, so regular use is not advised for people with heart conditions. A spirometry is also best not performed after a large meal (Mayo Clinic) or within six hours of the person having smoked (American Lung Association). In rare cases, the aggressive use of spirometry has led to pneumothorax (collapsed lungs) in people with emphysema.
Peak flow meters are useful for monitoring asthma but are not recommended for children under the age of 12 (Asthma Australia). Their usefulness as a diagnostic tool is also limited because it offers just one metric: The force with which a person is able to exhale.
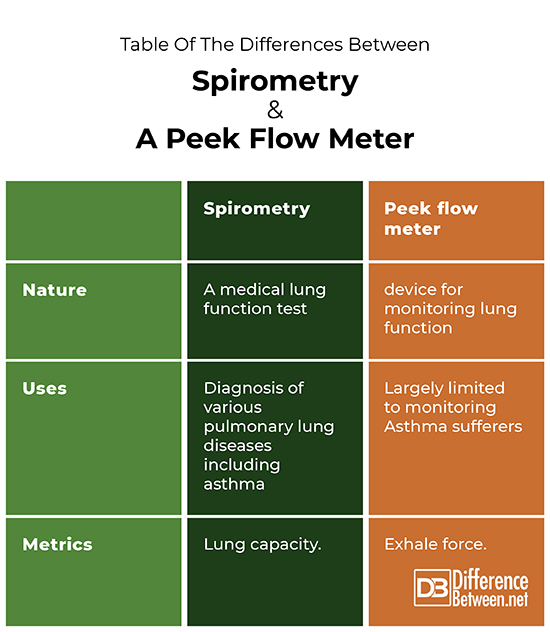
Table of the differences between spirometry and a peek flow meter
Summary
Spirometry, which is the test performed with a spirometer, offers a larger range of metrics for diagnosing lung health than does a peak flow meter, the metrics of which are limited to the force with which people exhale.
FAQ
Is a peak flow meter the same as spirometer?
Peak flow meters are not the same as spirometry. A peak flow meter is a device for monitoring lung function, while a spirometry is a test of lung functioning that can confirm a person has a lung disease (Asthma Australia). A spirometer is also a more sophisticated device and measures a wider variety of factors that include the peak exhale force, the forced expiration volume per second, forced vital capacity, as well as inspiration capacity (Andrew Gallagher).
What is the difference between a peak flow meter and an incentive spirometer?
An incentive spirometer is also a handheld device, but unlike a peak flow meter, it is designed to exercise the lungs and help keep them fluid free and strong. It is used to break up the fluid buildup in the lungs of people with pneumonia, patients subsequent to surgery, and patients suffering from lung illnesses. Breathing into an incentive spirometer raises a piston inside the device that measures the volume of air exhaled. A target breath volume can be set (ZeeNews), and patients can be taught to take slow, deep breaths to develop greater lung capacity (Deborah Leader) and prevent complications following pneumonia (Chin-Jung Liu, et al.). A peak flow meter can only monitor lung functioning; it cannot be used to exercise the lungs.
What is the difference between spirometry and PFT?
While both spirometry and peak flow tests are tests that assess a person’s lung functioning, spirometry is a diagnostic tool used by doctors to test lung capacity. Peak flow tests are performed by patients with device whose metric is limited to measuring the highest exhale force.
What is peak flow in spirometry?
Peak flow in spirometry is a measure of how forcefully a person can exhale over one second when exhaling into a spirometer.
Is a peak flow of 300 good?
Whether a peak flow of 300 is good would depend on a person’s personal best peak flow. To fall into the Green zone, which means the person is doing well, the person’s current peak flow can be as low as 241, but if their personal best is 375, they would need a current peak flow of at least 301 (Associated Allergists).
Are all peak flow meters the same?
Several brands of portable peak flow meters are available, all of which work in the same manner: A person blows fast, hard breath into a mouthpiece and records the score (Mayo Clinic). H. Koyama et al. compared the readings of four different brands and came to conclusion that “the limit of agreement between each PFM is so wide that we do not recommend the use of the readings of each meter interchangeably.”
- Difference Between Ecchymosis and Erythema - August 15, 2022
- Difference Between Autobiographical Memory and Episodic Memory - August 1, 2022
- Difference Between Biological Drive and Social Motive - July 30, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Associated Allergists and Asthma Specialists. Peak Flow Zone Chart. https://www.allergists-asthma.com/images/pdf/peak-flow-zone-chart.pdf.
[1]Cirno, Erica. “Spirometry Procedure: How to Prepare, Side Effects, and Risks.” Healthline. 2021. https://www.healthline.com/health/spirometry
[2]Koyama H., et al. “Comparison of Four Types of Portable Peak Flow Meters (Mini-Wright, Assess, Pulmo-Graph and Wright Pocket Meters).” Respiratory Medicine, 92(3):505-11, 1998. http://doi.org/10.1016/s0954-6111(98)90299-2.
[3]Liu, CJ, et al. Is Incentive Spirometry Beneficial for Patients with Lung Cancer Receiving Video-Assisted Thoracic Surgery? BMC Pulmonary Medicine, 19,121, 2019. https://doi.org/10.1186/s12890-019-0885-8
