Difference Between Necrotizing Fasciitis and Cellulitis
Necrotizing fasciitis is a bacterial infection that causes the necrosis of the fatty subcutaneous skin layer and the fascia which consists of the vasculature. This condition develops from blunt force tissue injury, open wounds, and from cellulitis. Cellulitis is a bacterial infection of the skin and soft tissue that results from a closed wound injury. Examples of such wounds include animal bites, burn injuries, diabetic ulcers, and surgical site infections.

What is necrotizing fasciitis?
Definition:
Necrotizing fasciitis also referred to as flesh-eating disorder, is an uncommon bacterial infection of subcutaneous tissue and fascia that causes the death of the tissue.
Risk factors:
Certain groups are at an increased risk of developing necrotizing fasciitis. These include diabetics, hypertensive individuals, obese patients, adults greater than 50 years old, those with cellulitis, immunocompromised individuals, those with liver or kidney failure, and those taking injectable medications.
Symptoms:
Early-onset necrotizing fasciitis has the following symptoms: pain out of proportion confined to one area of the body, fever, rapidly spreading erythema, and edema. Later on, the symptoms become more severe and include induration or stiffness of the involved body part, paresthesia, blackening and bruising of the skin, blistering and foul-smelling discharge, and septicemia.
Diagnosis:
Necrotizing fasciitis is difficult to diagnose. The symptoms are vague and not so apparent on the overlying skin. The important investigation includes an X-ray of the affected region which will confirm gas buildup. A computed tomography (CT) scan and a magnetic resonance imaging (MRI) scan are further carried out to determine the depth of necrosed tissue and biopsies of the affected area.
Treatment:
Necrotizing fasciitis is an aggressive infection that needs prompt treatment. Mortality rates are very high for the condition. Intravenous (IV) broad-spectrum antibiotics and IV fluid resuscitation are super important to control the infection. Dead tissue is removed via debridement surgery. Extensive excision of the debris is carried out. Sometimes, hyperbaric oxygen therapy (HBO) is in conjunction with antibiotics to promote rapid healing. Lastly, if the body part is unsalvageable, radical surgical intervention or amputation needs to be carried out.

What is cellulitis?
Definition:
Cellulitis is a bacterial infection of the skin and soft tissue that results from a closed wound injury. Examples of such wounds include animal bites, burn injuries, diabetic ulcers, and surgical site infections.
Risk factors:
The following group of people has an increased propensity to develop cellulitis: elderly patients, diabetics, those who have lymphedema, overweight patients, immunocompromised, those who have eczema, and those who have chickenpox or shingles.
Symptoms:
Symptoms of cellulitis include edema of the extremities, fever, hyperesthesia, redness, and induration. The affected limb is warm, tender, has blisters, and changes colors from time to time. The wound is often foul-smelling.
Diagnosis:
Cellulitis is diagnosed through physical examination. The signs and symptoms of cellulitis are distinct and often no blood tests are needed to confirm the condition.
Treatment:
Systemic antibiotics are the mainstay treatment for cellulitis. These dampen the bacterial overgrowth and aid the infected tissue healing. Surgical excision and skin grafts may be needed if the wound is large. Elevation of the affected limb helps resolve the swelling.
Difference between necrotizing fasciitis and cellulitis
Definition:
Necrotizing fasciitis is a bacterial infection that causes the necrosis of the fatty subcutaneous skin layer and the fascia which consists of the vasculature. Cellulitis is a bacterial infection of the skin and soft tissue that results from a closed wound injury.
Risk factors:
Necrotizing fasciitis is likely to develop in diabetics, hypertensive individuals, obese patients, adults greater than 50 years old, those with cellulitis, immunocompromised individuals, those with liver or kidney failure, and those taking injectable medications. Cellulitis is likely to develop in elderly patients, diabetics, those who have lymphedema, overweight patients, immunocompromised, those who have eczema, and those who have chickenpox or shingles.
Mortality rate:
Necrotizing fasciitis has a much higher mortality rate than cellulitis.
Location:
Necrotizing fasciitis involves the subcutaneous tissue and fascia whereas cellulitis is confined to the skin.
Speed of infection spreading:
Necrotizing fasciitis spreads rapidly as compared to cellulitis.
Diagnosis:
Necrotizing fasciitis is difficult to diagnose on physical examination. Radiologic investigations are needed to confirm the condition. Cellulitis is easily diagnosed on a physical exam.
Treatment:
Necrotizing fasciitis is treated with broad-spectrum IV antibiotics and fluid resuscitation, along with surgical debridement and sometimes amputation. Cellulitis is managed with systemic antibiotics and elevation of the affected region.
Prognosis:
The prognosis of necrotizing fasciitis is poor whereas the prognosis of cellulitis is good.
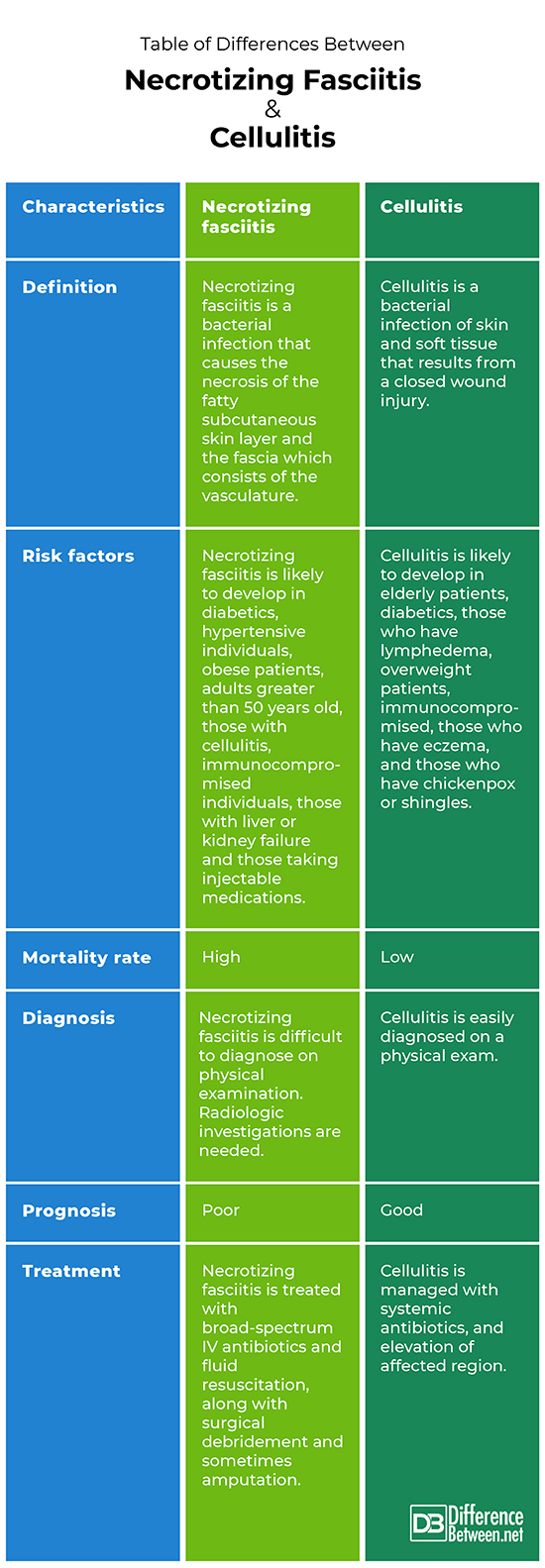
Table of differences between necrotizing fasciitis and cellulitis
FAQs:
Can cellulitis become necrotizing fasciitis?
If left untreated, cellulitis can progress to necrotizing fasciitis.
How do you rule out necrotizing fasciitis?
After physical examination, Xray and CT scan are carried out to confirm necrotizing fasciitis. Additionally, blood tests are also done.
What mimics necrotizing fasciitis?
Conditions such as non-necrotizing fasciitis, myositis, myonecrosis, and compartment syndrome mimic necrotizing fasciitis.
What does necrotizing cellulitis look like?
The skin affected in necrotizing fasciitis is initially pale, and later turns from red to orange to black.
Does cellulitis always lead to sepsis?
No. If not treated urgently with systemic antibiotics, cellulitis leads to sepsis.
What happens when cellulitis turns black?
Black tissue means it is dead and gangrenous. It cannot be salvaged.
How do you know if cellulitis is in your bloodstream?
Blood culture is needed to confirm septicemia.
What are the signs that cellulitis is getting worse?
The affected area has increasing pain, swelling, discharge and warmth.
What does severe cellulitis look like?
Worsening symptoms of pain, warmth, discharge and color changes indicate severe cellulitis.
- Difference Between Ocular Rosacea and Blepharitis - September 22, 2023
- Difference Between Toxic and Nontoxic Goiter - August 18, 2023
- Difference Between Anterolisthesis and Retrolisthesis - July 31, 2023
Search DifferenceBetween.net :
Leave a Response
References :
[0]Hayeri, Mohammad Reza, et al. "Soft-tissue infections and their imaging mimics: from cellulitis to necrotizing fasciitis." Radiographics 36.6 (2016): 1888-1910.
[1]Bouvet, A. "Cellulitis and necrotizing fasciitis: microbiology and pathogenesis." Annales de Dermatologie et de Venereologie. Vol. 128. No. 3 Pt 2. 2001.
[2]Green, Ronald J., Donald C. Dafoe, and Thomas A. Rajfin. "Necrotizing fasciitis." Chest 110.1 (1996): 219-229.
