Difference Between Celiac Disease and Ulcerative Colitis
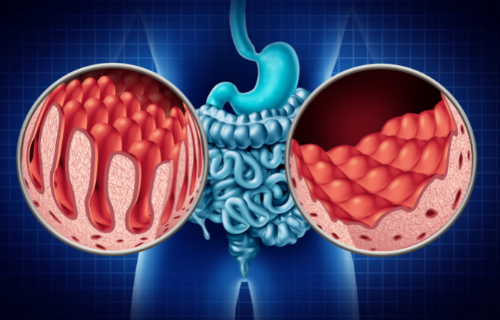
Ulcerative colitis is an inflammatory bowel disease (Celiac Disease Foundation) that causes ulcers in the digestive system and affects the innermost lining of the colon (large intestine) and rectum. It is a condition that develops over time (Mayo Clinic). Celiac disease is also a disease of the digestive system but is considered an autoimmune disorder that mostly affects the small intestine (Katri Lindfors et al.).
Causes
The causes of ulcerative colitis are unknown (Robert C. Langan et al.). Diet and stress may aggravate the condition but are not considered causes. Most people do not have a family history of ulcerative colitis, thus ruling out hereditary. One cause is thought to be an abnormal immune response to bacteria that results in the immune system attacking cells in the digestive tract.
In contrast, celiac disease is triggered by imbibing the protein gluten, which is found in grains like barley, wheat, and rye. Sensitivity to gluten leads to the immune system attacking the lining of the small intestine and the villi that absorbed nutrients (Cleveland Clinic).
Types and symptoms
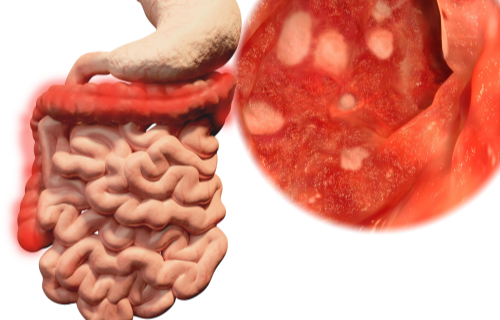
Ulcerative colitis is classified according to its location. There are four types:
- Ulcerative proctitis occurs in the area closest to the anus and is associated with rectal bleeding.
- proctosigmoiditis involves the rectum and sigmoid (lower section of the colon) and includes bloody diarrhea, abdominal cramps, and the inability to defecate;
- left-sided colitis involves the rectum, sigmoid, and descending colon and is associated with abdominal cramping, pain on the left side, urgency to defecate, and bloody diarrhea; and
- pancolitis affects the entire colon and includes abdominal cramps and pain, fatigue, and significant weight loss as well as severe bouts of bloody diarrhea.
The three types of celiac disease are classified according to their symptoms:
- Classic celiac disease presents with bouts of diarrhea between constipation, bloating, gas, anemia, a severe blistering skin rash and sores in the mouth, inflammation of the liver, muscle cramps and joint pain, and a tingling sensation in the legs. Long-term health complications include malnutrition, osteoporosis due to problems absorbing calcium and Vitamin D, infertility, and rarely, cancer of the intestine.
- Non-classic celiac disease, which according to the Cleveland Clinic is becoming the most common, presents only with anemia.
- Asymptomatic celiac disease presents with no symptoms at all.
Diagnosis
According to the Mayo Clinic, a tissue biopsy using endoscopic procedures (colonoscopy and flexible sigmoidoscopy) provide a definitive diagnosis for ulcerative colitis. Imaging procedures (X-ray, computerize tomography and magnetic resonance) may also be used to rule out serious complications like a perforated colon and establish where and how much of the colon is inflamed. To diagnose ulcerative colitis, other diseases of the digestive tract must be excluded, including Crohn’s disease, irritable bowel syndrome, bacterial infections of the colon, and colitis from other causes like medication.
In celiac disease, there are specific markers in the blood, namely, antibodies to gluten, which help with diagnosis as well as tests to identify nutritional shortages, for example, low levels of iron. A biopsy of the small intestine may be performed to check for damage to the villi (Katri Lindfors et al.).
Treatment
There is no known cure for ulcerative colitis (Mayo Clinic), and while not usually fatal, it is a serious disease that may cause life-threatening complications like severe bleeding and dehydration, a perforated colon, osteoporosis, inflammation of the eyes, joints, and skin, and increased risk of blood clots in the veins and arteries. It is also a colon cancer risk (Robert C. Langan et al.) In addition to anti-diarrheal medication, pain-relievers, antibiotics and immune system suppressors, anti-inflammatory medication such as steroids are used to treat the inflammation, and in some case, surgery.
Celiac disease is rarely fatal but because the villi that absorb nutrition are damaged, sufferers may end up with malnutrition (Cleveland Clinic). A gluten-free diet improves the condition almost immediately, but the villi take time to heal and straying from a strictly gluten-free diet may reactivate the condition.
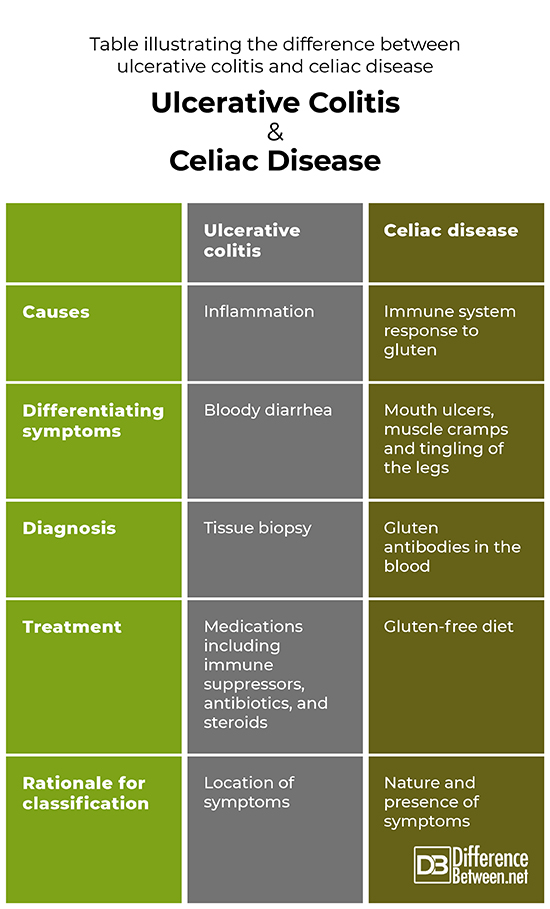
Table illustrating the difference between ulcerative colitis and celiac disease
Summary
Ulcerative colitis and celiac disease are both diseases of the digestive system, but the former is an inflammatory condition and the latter an autoimmune response to a gluten sensitivity. The presence of bloody diarrhea implies ulcerative colitis, but a firm diagnosis requires a tissue biopsy and treatment involves medication and even surgery. Celiac disease can be diagnosed by the presence of gluten antibodies in the blood and is treated with gluten-fee diet.
FAQ
Can celiac disease be confused with ulcerative colitis?
While celiac disease and ulcerative colitis are both diseases of the digestive system that are associated with abdominal discomfort, they present with symptoms that would differentiate them. The presence of bloody diarrhea points to celiac disease. The presence of symptoms beyond the digestive tract, for example, muscle cramps, joint pains, and tingling in the lower extremities, suggests ulcerative colitis as opposed to celiac disease.
Is colitis the same as celiac disease?
Colitis is classified as an inflammatory bowel disease and considered serious, whereas celiac disease is the result of an immune system response to gluten that damages the villi in the small intestine. Inflammation is rare is celiac disease.
Can gluten cause ulcerative colitis?
A sensitivity to gluten that activates the immune system that then attacks the villi responsible for absorbing nutrients is considered the primary cause of ulcerative colitis.
How can you tell the difference between celiac and Crohn’s?
Both celiac and Crohn’s diseases point to intestinal inflammation and share the symptoms of abdominal pain and diarrhea, and Crohn’s disease is more likely to manifest among those who already have celiac disease (Yang et al.). What differentiates celiac from Crohn’s disease is that in celiac disease inflammation is limited to the colon, whereas in Crohn’s disease, chronic inflammation occurs anywhere from the mouth to the anus.
- Difference Between Ecchymosis and Erythema - August 15, 2022
- Difference Between Autobiographical Memory and Episodic Memory - August 1, 2022
- Difference Between Biological Drive and Social Motive - July 30, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Celiac Disease Foundation. About Celiac Disease, 2021, https://celiac.org/about-celiac-disease/
[1]Cleveland Clinic. Celiac Disease, 2020, https://my.clevelandclinic.org/health/diseases/14240-celiac-disease#symptoms-and-causes
[2]Langan, Robert C. et al. Ulcerative colitis: diagnosis and treatment," American Family Physician, 2007, Nov 1, 76 (9):1323-1330.
[3]Lindfors, Katri et al. Coeliac disease. Nature Reviews Disease Primers, 2019, Dec., 5 (1): 3 https://doi.org.10.1038/s41572-018-0054-z
[4]Mayo Clinic. Ulcerative colitis, 2022, https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis
[5]Yang A. et al. Inflammatory bowel disease in patients with celiac disease. Inflammatory Bowel Disease in Patients, 2005, 11: 528-532. http://celiacdisease.sklad.cumcweb.org/sites/default/files/2005-Inflammatory-Bowel-Disease-in-Patients-With-Celiac-Disease.pdf
