Difference Between Outpatient Coding and Inpatient Coding
The hospital coding and billing is indeed a complex system considering the complexity of the hospital environment. Thousands of individuals are employed at a hospital facility to make sure everything at the facility is well organized and systematic – staring from patient billing process to the reimbursement process. It’s a challenge in itself making sure patient billing process is done and successful reimbursement is claimed at a timely manner.
Coding serves a number of purposes including retrieving and reporting information on the basis of diagnosis and procedure. However, coding involves much more than just the systematic assignment of codes. More complex is the documentation that it follows.
The patient’s medical record is the foundation for coding. And the golden rule of coding is proper documentation. It’s a term used to describe information regarding the patient’s condition, treatment, and response to treatment. Based on whether a patient is an outpatient or an inpatient, the medical codes vary differently. And it’s the role of a certified coder to review medical records of patients and then assign codes to their diagnoses.
Coding basically involves assigning numeric or alphanumeric codes to all healthcare data elements of outpatient and inpatient care. So, one of the most important key aspects of hospital coding and billing process is to identify whether the patient is an outpatient or an inpatient.
What is Outpatient Coding?
Outpatient refers to a patient who is being treated but not admitted under the care of the hospital for an extended stay and is released from the hospital within 24 hours. Even if a patient stays for over 24 hours, he/she can be considered an outpatient. The outpatient coding is based on the ICD-9/10-CM diagnostic codes for billing and appropriate reimbursement, but uses CPT or HCPCS coding system to report procedures. Documentation plays a crucial role in the CPT and HCPCS codes for services.

What is Inpatient Coding?
Inpatient refers to a patient who is formally admitted to a hospital upon the orders of the physician who then admits the patient for an extended stay. The inpatient coding system is used to report a patient’s diagnosis and services based on his extended stay. It also uses ICD-9/10-CM diagnostic codes for billing and appropriate reimbursement but uses ICD-10-PCS as the procedural coding system. The Inpatient Prospective Payment System (IPPS) is the reimbursement methodology used by Medicare to provide reimbursement for hospital inpatient services.

Difference between Outpatient and Inpatient Coding
Basics of Outpatient Vs. Inpatient Coding
Outpatient refers to a patient who checks into the ER and is being treated but is not admitted to the hospital for an extended stay. The patient is usually released from the hospital the same day within 24 hours. When a patient is formally admitted to a hospital upon the physician’s orders who then take care of your extended stay at the hospital stay, he is considered an inpatient. Outpatient coding refers to a detailed diagnosis report in which the patient is generally treated in one visit, whereas an inpatient coding system is used to report a patient’s diagnosis and services based on his extended stay.
Coding for Outpatient Vs. Inpatient
The inpatient coding system is solely based on the assignment of ICD-9/10-CM diagnostic and procedural codes for billing and appropriate reimbursement. It’s the standard coding system used by physicians and other healthcare providers for classification and coding of all diagnoses. It uses ICD-10-PCS to report procedures. The process of the locating the appropriate ICD-9/10-CM diagnostic codes remains the same for outpatient services but the outpatient facility services are reimbursed based on the code assignments from the CPT (Current Procedural Terminology) and HCPCS (Healthcare Common Procedure Coding System)coding system. Documentation plays a crucial role in the CPT and HCPCS codes for services.
Principal Diagnosis
The principal diagnosis is defined as the condition established after study that is solely responsible for admittance of the patient under the care of the hospital. The principal diagnosis is sequenced first in inpatient coding. The correct assignment of an appropriate principal diagnosis determines whether payment is made thoroughly. In short, the principal diagnosis is the key in determining the resources required by a patient. The term principal diagnosis, however, is not utilized for outpatient purposes as the diagnoses are often not established at the time of the first visit, so in many instances the first-listed condition is used to indicate the main reason of the visit.
Payment involved in Outpatient Vs. Inpatient Coding
The Inpatient Prospective Payment System (IPPS) is the reimbursement methodology used by healthcare providers and government programs to provide reimbursement for hospital inpatient services based on the patient’s diagnosis and treatment provides during his/her hospitalization. The patients are grouped under diagnosis related groups (DRGs) based on clinically similar patients or patients who share similar hospital resources. Outpatient Prospective Payment System (OPPS), on the other hand, is a prospect payment system that provides reimbursement for hospital outpatient services. The system implemented under this payment system is known as Ambulatory Payment Classifications.
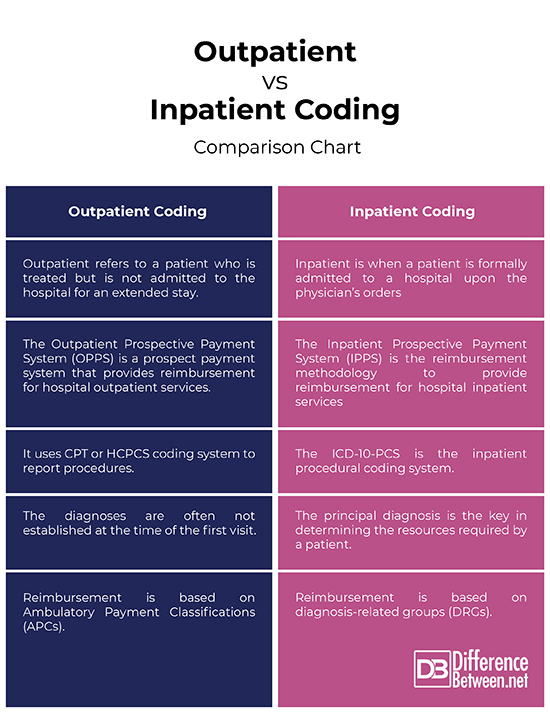
Outpatient vs. Inpatient Coding: Comparison Chart
Summary of Outpatient Vs. Inpatient Coding
In a nutshell, the groundwork remains the same but the coders need to keep up-to-date with the changing hospital coding regulations in compliance with both the inpatient guidelines and outpatient guidelines. The hospital facility offers a host of settings that involve claiming services and billing and coding appropriately for reimbursement. Hospital size is often measured by the number of inpatient admissions possible or number of beds available for inpatient care. Rest is on the coders because codes vary from hospital to hospital and physician to physician. Likewise, inpatient coding is very different from outpatient coding in terms of approach, guidelines, payment system, and so on.
- Difference Between Caucus and Primary - June 18, 2024
- Difference Between PPO and POS - May 30, 2024
- Difference Between RFID and NFC - May 28, 2024
Search DifferenceBetween.net :
Leave a Response
References :
[0]Ferenc, Debra P. Understanding Hospital Billing and Coding. NYC: Elsevier, 2013. Print
[1]Diamond, Marsha. Understanding Hospital Coding and Billing: A Worktext. Boston: Cengage, 2015. Print
[2]Image credit: https://www.health.mil/-/media/Images/MHS/Photos/cold--flu-season.ashx?h=428&la=en&mw=720&w=720&hash=A99102393036BE60119B1D1CB4FB7E0D7DC09F61
[3]Image credit: https://media.defense.gov/2009/Jun/01/2000562024/-1/-1/0/090529-F-5342S-262.JPG
