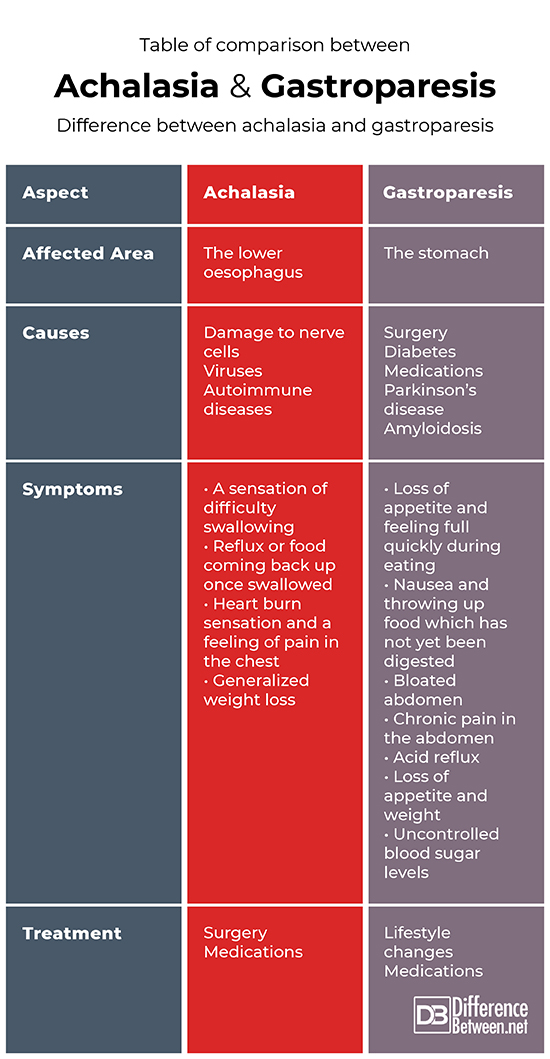
Difference Between Achalasia and Gastroparesis
Gastroparesis and achalasia are both intestinal motility disorders. The term “intestinal motility disorders” commonly means abnormal intestinal contractions, for instance spasms or sometimes intestinal paralysis. This term is used to describe a different disorder in which the gut has lost its ability to synchronize muscular activity properly.
The two conditions are closely related, although one involves the oesophagus and the other involves the stomach. They both present with symptoms which are very similar and can overlap, however, there are distinctive signs differentiating to two from one another.
Both gastroparesis and achalasia can be treated, and the results show a positive future for the patients.

This article takes a close look at what truly differentiates the two conditions.
Definition
Achalasia
Achalasia is defined as an oesophageal motility disorder of primary type.
It is generally characterized by the absence of oesophageal peristalsis (muscle contractions) and an improper relaxation of the lower oesophageal sphincter (the muscle at the bottom of the oesophagus) in relation to swallowing motions. In fact, the lower oesophageal sphincter muscle is seen to be in a hyper tensed state in half of the patients suffering from this condition.
This abnormal function can lead to a blockage further down at the gastroesophageal junction.
Gastroparesis
Gastroparesis refers to the partial paralysis of the stomach. It is a disease where the stomach is unable to empty the food out of itself in a normal manner. Gastroparesis happens when damaged nerves and muscles simply cannot function to their normal capacity and end up severely slowing down the movement of stomach contents throughout the digestive system.
Causes and Symptoms
Achalasia
The pinpoint causes of achalasia are unknown to medical professionals. It is suspected that a loss of nerve cells in the oesophagus are what causes this condition. Other causal factors such as viruses and autoimmune diseases are also suspected by research specialists.
Symptoms often include:
- A sensation of difficulty swallowing
- Reflux or food coming back up once swallowed
- Heart burn sensation and a feeling of pain in the chest
- Generalized weight loss
Gastroparesis
Gastroparesis is often a complication following intestinal or gastric surgery. Other causes include diabetes disease and even pain medication induced gastroparesis. On rare occasions, gastroparesis is seen in patients suffering Parkinson disease and amyloidosis.
Symptoms of gastroparesis may include:
- Loss of appetite and feeling full quickly during eating
- Nausea and throwing up food which has not yet been digested
- Bloated abdomen
- Chronic pain in the abdomen
- Acid reflux
- Loss of appetite and weight
- Uncontrolled blood sugar levels
Diagnosis
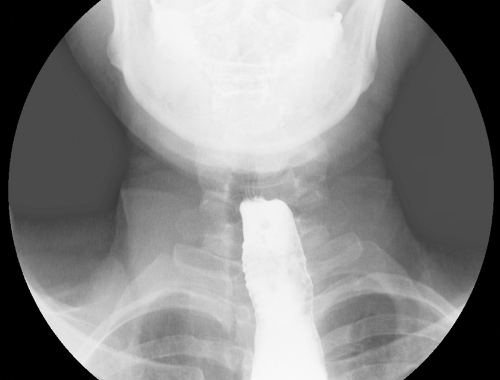
Typical tests done to done to diagnose achalasia include endoscopy (scoping the oesophagus) where results show no presence of a blockage. A barium swallow x-ray test can also be done. This diagnosis should be made based on the above-mentioned medical tests and the presence of symptoms in the patient.
The diagnosis for gastroparesis is done by a gastric emptying scan. To do this scan, the patient will eat food (such as eggs) that are mixed into a safe radioisotope (radioactive substance). This substance will present when the patient is scanned in an imaging machine and measures how the food leaves the stomach. If over half of the food stays in the stomach for an hour after eating, then a diagnosis of gastroparesis is made.
An additional test called manometry can be done and this will measure how well the stomach contractions are taking place.
Treatment and Prognosis
Achalasia
Achalasia is treated by focusing on relaxing the lower part of the oesophagus through medications. Surgical stretching of the lower oesophagus is also often done by specialist surgeons. This will allow the food or liquid to travel through the digestive passage with ease.
The surgical procedures include pneumatic dilation – where a balloon is placed through the oesophagus and inflated to stretch the affected area. Botox can be injected into the oesophageal sphincter muscle directly to relax and paralyze it.
The majority of patients who are correctly treated can live a relatively normal life. Unfortunately, the disease has a tendency to occur again but can be treated just as effectively.
Gastroparesis
Gastroparesis is treated primarily with dietary habits. These include eating smaller portions and not eating any food that is tough to digest (such as citrus fruit and fatty food). Medication can also be prescribed to patients and helps the stomach to empty itself more quickly.
Patients suffering from gastroparesis can live a normal life. However, the conditions does tend to cause complications and reduce a patient’s quality of life.
Table of comparison between
Summary
Regarding the mechanism of the diseases and the symptoms, achalasia and gastroparesis are very similar. Both conditions involve paralysis of muscular structures in the gastrointestinal tract with shared symptoms such as nausea, vomiting and heartburn. Both conditions require diagnosis and treatment by a medical specialist.
When treated correctly from both the medical professional and commitment from the patient, these conditions can be well controlled.
FAQ
Does achalasia cause gastroparesis?
Achalasia does not cause gastroparesis and as they are two completely separate medical diagnoses. Although they share many similarities, there is absolutely no association between achalasia and gastroparesis.
What can be mistaken for gastroparesis?
Gastroesophageal reflux disease often closely mimics gastroparesis and can be mistaken for it.
What is the difference between achalasia and dysphagia?
Dysphagia is defined as difficulty swallowing. Dysphagia is a symptom of achalasia and is not a disease on its own.
What can mimic achalasia?
There are other motility disorders of the esophagus such as diffuse esophageal spasm that may have similar symptoms to achalasia but are a different medical condition.
- Difference Between a Cochlear Implant and Normal Hearing - October 4, 2022
- Difference Between Obstructive and Restrictive Spirometry - September 11, 2022
- The Difference Between White Box and Black Box Testing - September 11, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Di Lorenzo, C. & Youssef, N. “Diagnosis and management of intestinal motility disorders”. Seminar of Paediatric Surgery, vol. 19, no. 1, 2010, pp: 50-58.
[1]Di Lorenzo, C. & Youssef, N. “Diagnosis and management of intestinal motility disorders”. Seminar of Paediatric Surgery, vol. 19, no. 1, 2010, pp: 50-58.
[2]Gyawali, C. “Achalasia: new perspectives on an old disease”. Neurogastroenterological Motility, vol. 28, no. 1, 2016, pp:4-11.
[3]Mayo Clinic. “Achalasia”. https://www.mayoclinic.org/diseases-conditions/achalasia/diagnosis-treatment/drc-20352851
[4]University of California San Francisco. “Gastroparesis Treatments”. https://www.ucsfhealth.org/conditions/gastroparesis/treatment
