Difference Between Narcolepsy Brain and Normal Brain
Narcolepsy, also called “sleep attacks,” is a chronic neurological disorder involving the brain’s control of a person’s sleep and wakefulness patterns. Approximately one in 2,000 Americans suffer from narcolepsy. The condition affects an equal number of males and females (Cleveland Clinic).
Narcolepsy includes three types:
- Type 1 narcolepsy is characterized by excessive daytime sleepiness with cataplexy and/or low levels of hypocretin.
- Type 2 narcolepsy is characterized by excessive daytime sleepiness, the absence of cataplexy, and normal levels of hypocretin (Cleveland Clinic).
- Secondary narcolepsy is often a result of injury to the hypothalamus, an area in the brain that assists with regulating sleep. In addition to the typical symptoms of narcolepsy, secondary narcolepsy may include severe neurological problems and excessive sleeping (more than 10 hours) each night (NINDS).
Narcolepsy exhibits the following symptoms:
- Daytime sleepiness, which includes mental cloudiness or “brain fog” and associated cognitive impairments (Soo-Me Yoon), including lack of concentration and memory lapses, as well as depressed mood and low energy and/or extreme exhaustion (Cleveland Clinic).
- About 70% of those affected with narcolepsy experience a sudden loss of muscle strength, known as cataplexy. Cataplexy may be mistaken for seizures (NINDS) and can last from a few seconds to several minutes. The person remains conscious during these attacks. The rate of attacks can range from a few in a lifetime to several a day (Cleveland Clinic).
- Sleep paralysis is characterized by the inability to move or speak prior to falling asleep or upon awakening. Episodes last from seconds to a few minutes.
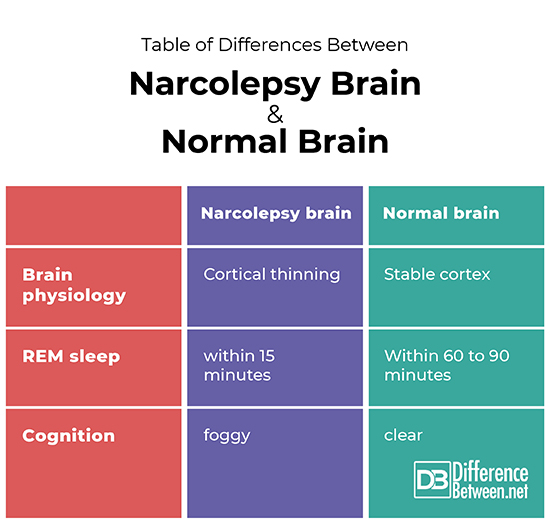
- The condition often includes disrupted sleep or frequent awakening during the night (Cleveland Clinic) as well as rapid entry into the dream state. Normally, a person enters rapid eye movement (REM) sleep after about 60 to 90 minutes and begins to dream; people with narcolepsy, however, often enter REM sleep within 15 minutes of falling asleep. During the REM state, the brain keeps a person’s muscles limp to prevent the person acting out their dreams. This function can be absent for the narcoleptic sufferer, while the REM state can occur during wakefulness. Sleep may also be disrupted by insomnia, vivid dreaming, and sleep apnea (NINDS).
- The narcoleptic might also experience vivid fearful hallucinations that occur just before falling asleep (hypnagogic hallucinations) or just after awakening (hypnopompic hallucinations). Hallucinations are most often visual but can involve all the senses (Cleveland Clinic).
- Automatic behavior describes how the person falls asleep for several seconds but continues to perform routine tasks without awareness or memory of having done the task (Cleveland Clinic).
Causes
Over the last 20 years, some progress has been made with respect to understanding the causes of narcolepsy. One explanation is genetic and points to the activity of groups of neurons in several parts of the brain that interact to control sleep (Cleveland Clinic).
A related explanation is the loss of a neurotransmitter, specifically hypocretin. Hypocretin is important for regulating the sleep/wake cycle including the rapid eye movement (REM) during the sleep state. A shortage of hypocretin causes excessive sleepiness, and features of REM sleep (also called “dreaming sleep”) become present during wakefulness (Lisa Spear; NINDS). When these neurons disappear, changes between wakefulness, REM sleep, and non-REM sleep can happen spontaneously, resulting in sleep fragmentation and the daytime symptoms people with narcolepsy experience. This is considered the primary cause of type 1 narcolepsy.
Scientists are unsure about why hypocretin neurons die. Some suggest narcolepsy is due to autoimmune disorder that attacks the brain cells that produce hypocretin because of higher-than-normal levels of anti-streptolysin O antibodies in people with narcolepsy. The seasonal onset of narcolepsy confirms the autoimmune system explanation: People are more likely to develop symptoms after the winter season. The H1N1 influenza epidemic in 2009, for example, was associated with an increase in the onset of cases of narcolepsy (NINDS).
Family history also plays a part. About 10% of people with narcolepsy have close relatives with similar symptoms, while environmental toxins, such as secondhand smoke, heavy metals, and the presence of pesticides, may contribute (Cleveland Clinic).
In rare instances, narcolepsy may result from injury to the area of the brain that controls REM sleep and wakefulness, for example, trauma, disease, or tumors in those regions (NINDS).
Diagnosis and Treatment
Diagnosis is made based on symptoms and sleep studies after first ruling out other physical disorders (apnea, anemia, heart failure), mental disorders (major depression), and behavioral disorders (drinking alcohol and not getting enough sleep), which are also associated with excessive daytime sleepiness (NINDS).
Medications used to treat narcolepsy include wake- and sleep-promoting medications such as stimulants and antidepressants. Lifestyle changes include removing electronic devices from the bedroom, avoiding heavy meals and stimulants several hours before bedtime, exercising early in the day, relaxing before bedtime, and establishing a regular sleep/wake pattern. When suffering from narcolepsy, a person is advised not to drive or to nap before driving, drive short distances at a time, and keep engaged while driving (Cleveland Clinic).
Table of differences between narcolepsy brain and normal brain
Summary
Narcolepsy, also called “sleep attacks,” is a chronic neurological disorder in which a person is unable to control their sleep and wakefulness patterns. Symptoms include excessive daytime sleepiness, cataplexy, sleep paralysis, disrupted sleep, hallucinations, and automatic behavior. Scientists have considered genes, the loss of a neurotransmitter called hypocretin, and autoimmune responses to a variety of pathogens as responsible for the condition.
FAQ:
Does narcolepsy damage the brain?
Structural changes that include widespread and progressive cortical thinning as people with narcolepsy age have been noted (S. Jeon et al.; Lisa Spear). The prefrontal cortex, responsible for executive functions, memory, cognition, and emotions, as well as the hippocampus, are affected. Those with type 1 narcolepsy have a die-off of hypothalamic neurons that produce hypocretin, which regulates wakefulness and muscle tone.
How narcolepsy messes with your brain?
The relationship between narcolepsy and Lewy Body dementia is not well established but research suggests that hypocretin/orexin levels are low in those with Lewy-Body Dementia. Narcolepsy presenting in the elderly may therefore be a precursor to Lewy Body dementia (Stanley Thomas and Salman).
Can narcolepsy affect intelligence?
A study by So-Mee Yoon et al. noted that narcolepsy patients with a high IQ exhibit significant cognitive impairment and have deficits in visual attention and visual working memory.
Does narcolepsy affect thinking?
Narcolepsy appears to affect sufferer’s cognitive or thinking functions in so much as they experience mental fogginess, poor memory, and hallucinations (Sleep Review).
- Difference Between Ecchymosis and Erythema - August 15, 2022
- Difference Between Autobiographical Memory and Episodic Memory - August 1, 2022
- Difference Between Biological Drive and Social Motive - July 30, 2022
Search DifferenceBetween.net :
Leave a Response
References :
[0]Cleveland Clinic. Narcolepsy. 2020. https://my.clevelandclinic.org/health/diseases/12147-narcolepsy#:~:text=Scientists%20have%20discovered%20that%20people,movement%20(REM)%20sleep%20state.
[1]Jeon S, J.W. Cho, H. Kim, A.C. Evans, S.B. Hong, and E.Y. Joo. “A Five-Year Longitudinal Study Reveals Progressive Cortical Thinning in Narcolepsy and Faster Cortical Thinning in Relation to Early-Onset. Brain Imaging Behavior, vol. 14, no. 1: 200-212. Feb 2020. https://doi.org/10.1007/s11682-018-9981-2.
[2]National Institute of Neurological Disorders and Stroke. Narcolepsy Fact Sheet. April 25, 2022. https://www.ninds.nih.gov/health-information/patient-caregiver-education/fact-sheets/narcolepsy-fact-sheet.
[3]Sleep Review. For People with Narcolepsy, ‘Brain Fog’ May Be Debilitating Symptom.
[4]Dec 20, 2014. https://sleepreviewmag.com/sleep-disorders/hypersomnias/narcolepsy/narcolepsy-brain-fog-debilitating-symptom/#:~:text=Excessive%20daytime%20sleepiness%20(EDS)%20is,brain%20fog%E2%80%9D%20among%20narcolepsy%20patients.
[5]Spear, Lisa. “How Does Narcolepsy Change the Brain over Time?” Sleep Review. Dec 21, 2018. https://sleepreviewmag.com/sleep-disorders/hypersomnias/narcolepsy/narcolepsy-brain/Childhood disease onset linked to faster cortical thinning.
[6]Thomas, Stanley and Salam Salman. “1114 Lewy Body Dementia Initially Presenting as Narcolepsy.” Sleep, vol. 41 (Suppl. 1), April 2018, pp. A413–A414. https://doi.org/10.1093/sleep/zsy063.1113.
[7]Yoon, So-Mee et al. “Is High IQ Protective Against Cognitive Dysfunction in Narcoleptic Patients?” Journal of Clinical Neurology (Seoul, Korea) vol. 9, no. 2, 2013: 118-24. doi:10.3988/jcn.2013.9.2.118.
